Blocked Tear Ducts – Kids (Probing/Tubes)
What Do Tears Do, and Where Do They Go?
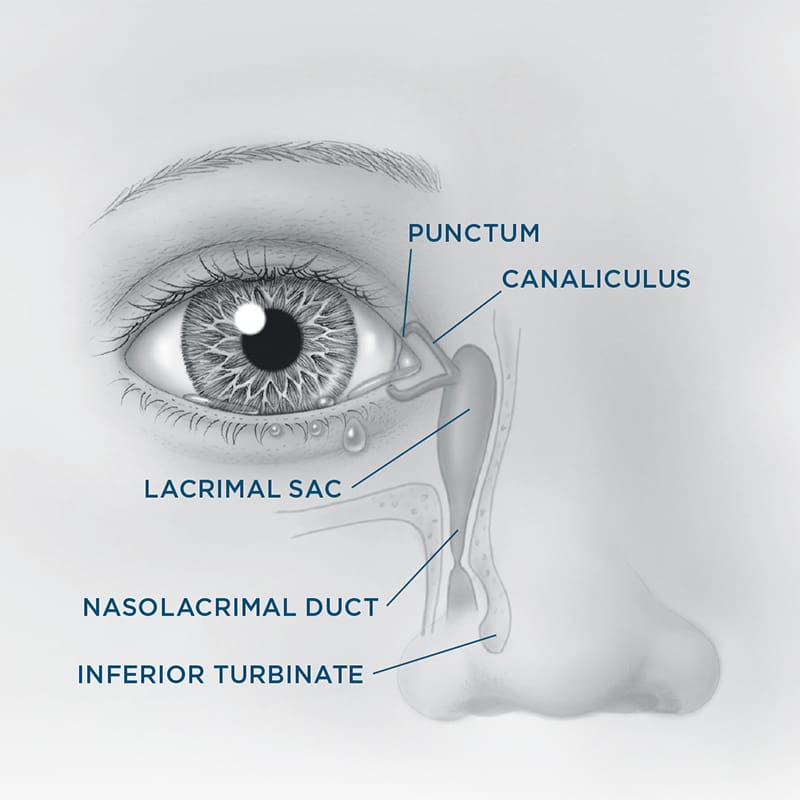
Tears keep your child’s eyes healthy and comfortable. Tear glands make small amounts of moisture all day, which spreads across the eyes every time your child blinks. Old tears normally drain through a tiny system that starts in the inner corners of the eyelids and empties into the nose.
The tear drain system includes:
• Puncta: Tiny openings in the upper and lower eyelids
• Canaliculi: Small tubes that carry tears into the lacrimal sac
• Lacrimal sac: A small space between the eye and nose
• Nasolacrimal duct: A narrow passage that leads from the sac into the nose
Blinking helps pump old tears through this system and into the nasal cavity.

What Is a Blocked Tear Duct?
About 7% of babies are born with a blocked tear duct, and it’s more common in premature infants. In most cases, the blockage is caused by a thin membrane at the bottom of the nasolacrimal duct, which keeps tears from draining into the nose.
If the tears can’t drain, they back up and may cause:
• Constant watering or tears running down the cheek
• Mucus or discharge
• Irritation or redness
• Swelling near the inside corner of the eye
Sometimes, tears trapped in the drainage system can become infected. While blocked tear ducts are the most common cause of tearing in babies, other causes are possible. It’s important that an oculofacial plastic surgeon examines your child to confirm the diagnosis.
Treatments Options
Conservative Treatment (First Year of Life)
Most blocked tear ducts clear up on their own by the time a child turns one. Your child’s doctor may recommend:
• Gently massaging the area near the tear sac several times a day
• Antibiotic drops, ointment, or oral medication if there’s discharge
Probing Procedure
If the duct stays blocked, your doctor may recommend a probing procedure. A thin metal probe is inserted into the punctum and passed down the tear duct to open the blockage. This is a short outpatient procedure and may be done in the office or operating room.
Other Options for More Severe Cases
In more persistent or complex cases, other procedures may be recommended:
• Balloon dilation to gently widen the duct
• Placement of a small temporary silicone stent to keep the duct open
• Surgery to create a new drainage pathway (rare)
Most children feel little to no discomfort after these treatments, and symptoms usually improve quickly.
Risks and Complications
All procedures carry some risks, but serious problems are uncommon. Possible side effects include:
• Minor swelling or bruising around the eye (usually resolves in 1–2 weeks)
• Bleeding or infection (rare)
• Scar tissue that could block the duct again and require another procedure
No surgical outcome is guaranteed. Your child’s surgeon will explain the risks and help you understand all available options.
Summary
Blocked tear ducts are common in infants and often clear up with time and simple care. When needed, procedures like probing or stenting can usually resolve the problem with minimal discomfort. Your oculofacial plastic surgeon will recommend the best approach based on your child’s age and symptoms.